Vaccines consistently transform public health, and HIV vaccine research has been a pillar of NIAID’s scientific mission since the beginning of the HIV pandemic. An HIV vaccine has proven to be among the most daunting scientific challenges, but has inspired exceptional innovation and collaboration in all aspects of our research approach. On the 27th observance of HIV Vaccine Awareness Day (Saturday, May 18), we express our gratitude to the dedicated global community of scientists, advocates, study participants, study staff, and funders working toward a safe, effective, durable, and accessible HIV vaccine.
As the lead of the National Institutes of Health HIV vaccine research effort, NIAID conducts basic, preclinical, and clinical research to characterize the safety, immunogenicity, and efficacy of promising HIV vaccine concepts. Through the HIV Vaccine Trials Network, NIAID supports clinical trials where HIV is most prevalent, including in the Global South. Over decades of research, with disappointing results from large efficacy studies, the HIV vaccine field has learned and iteratively evolved with every step. We have more knowledge now than ever before about how an HIV vaccine could work. Research teams are using discovery medicine trials and new vaccine technologies to identify and stimulate the types of immune responses that hold the most promise for preventing HIV.
People with HIV have made priceless contributions to HIV vaccine science by participating in research that teaches us how the human immune system responds to HIV. Some people naturally keep the virus under control even without antiretroviral therapy. Through their participation in clinical research, we have identified aspects of both cellular immunity—which is driven by T cells—and humoral immunity—driven by antibody-producing B cells—that likely will need to be stimulated and substantially amplified by a safe and effective preventive vaccine.
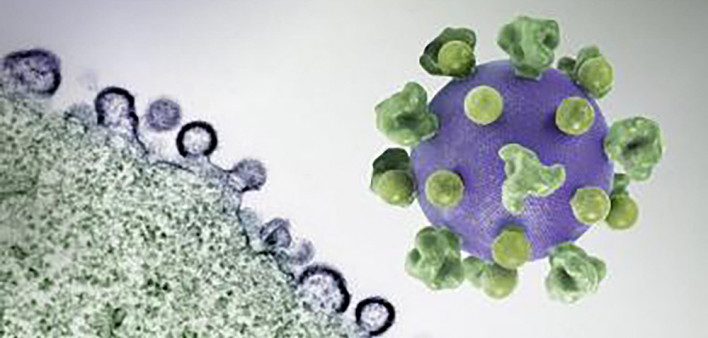
HIV’s genetic diversity makes it difficult to target with a vaccine, but broadly neutralizing antibodies (bNAbs) may be key to overcoming that hurdle because they bind to parts of the virus that are relatively consistent among variants. The NIAID Vaccine Research Center (VRC)—founded to accelerate HIV vaccine research on this day in 1997—isolated and then manufactured a bNAb called VRC01 that has prompted a cascade of other research, including HIV vaccine and passive antibody administration studies.
Since the VRC’s discovery of VRC01, scientists have identified additional bNAbs that target other stable sites on HIV’s highly variable surface. This year, VRC scientists showed that a human bNAb called VRC34.01, which targets the fusion peptide on HIV’s surface, protected monkeys from acquiring simian-HIV in a proof-of-concept study that is informing human vaccine design. Researchers at the VRC and other NIAID-supported institutions are using a technique called germline targeting to closely guide naïve (new) B cells to develop into mature B cells that can produce bNAbs. Using this approach, researchers are making progress toward eliciting VRC01-like antibodies, as well as several other classes of bNAbs in human and animal studies.
Researchers also are advancing cellular immune approaches to HIV vaccines. A study conducted by NIAID’s Laboratory of Immunoregulation found that a safe and effective HIV vaccine will likely need to stimulate strong responses from CD8+ T cells. NIAID and its partners announced the launch of a clinical trial to examine the safety and immune response generated by VIR-1388, a T-cell based vaccine candidate that uses a cytomegalovirus (CMV) vector. In this approach, a weakened version of CMV delivers HIV vaccine material to the immune system without causing disease in the study participants. The CMV vector technology has been in development with NIAID funding since 2004.
We also are reminded how HIV vaccine research and discovery benefits the broader fields of immunology and vaccinology. In October 2023, the Nobel Prize for Physiology or Medicine was awarded to Drew Weissman, MD, PhD, and Katalin Karikó, PhD, for their work that enabled the unprecedented rapid development of the mRNA vaccines that stemmed the COVID-19 pandemic and saved millions of lives. Both Nobel laureates have connections to NIAID and NIH. This research was made possible in part by NIAID HIV vaccine research grants that enabled a major evolution in understanding how immune cells recognize and react to different forms of mRNA. mRNA-based HIV vaccine candidates are now being tested in humans in early-stage trials.
Looking ahead, NIAID has clear priorities for HIV vaccine research and development. Ongoing research is guiding the next steps in vaccine strategies to elicit bNAbs and T-cell responses, to eventually trigger both with a single vaccine regimen. To enhance the precision of this research, more information is needed to define the correlates of protection for an HIV vaccine, that is, the specific immunologic markers that translate to a protective effect. Meanwhile, as promising concepts are identified and advanced through clinical trials, the field must continue to optimize vaccine formulations and dosing, and find novel adjuvants that can prolong and amplify immune responses. HIV vaccine research findings will continue to offer valuable insight in other areas, including HIV prevention and cure research, and broader medical countermeasure development for pandemic preparedness.
The pursuit of an HIV vaccine depends on supporting next the generation of HIV clinical investigators and community leaders. NIAID is committed to fostering the professional growth of early-stage HIV investigators and to nurturing the decades-long community partnerships that make this essential research possible.
On this HIV Vaccine Awareness Day, we remain optimistic that exciting scientific advances and the efforts of diverse partners around the world will put a safe and effective HIV vaccine within our grasp.
This NIAID News blog post was published by the National Institute of Allergy and Infectious Diseases on May 16, 2024.





Comments
Comments